Efforts to improve Canada’s organ donation and transplantation system have increased over the last 20 years. However, despite a significant increase in the number of organ transplants conducted in Canada between 2009 and 2018, the supply of organs does not meet demand, and thousands of individuals are on a waiting list for transplants. Moreover, many Canadians on the waiting list die before appropriate organs become available.
Deceased organ donors can provide up to eight organs for transplant, although the average number of organs used for transplantation in Canada is three to four organs per donor. Living donors provide a single organ – most commonly a kidney or part of a liver. There were 762 deceased organ donors in Canada in 2018, and the deceased organ donor rate increased by 42% between 2009 and 2018. In 2018, there were 555 living donors. Although the rate of organ donation by living donors increased between 2003 and 2011, the rate decreased by 2% between 2009 and 2018.
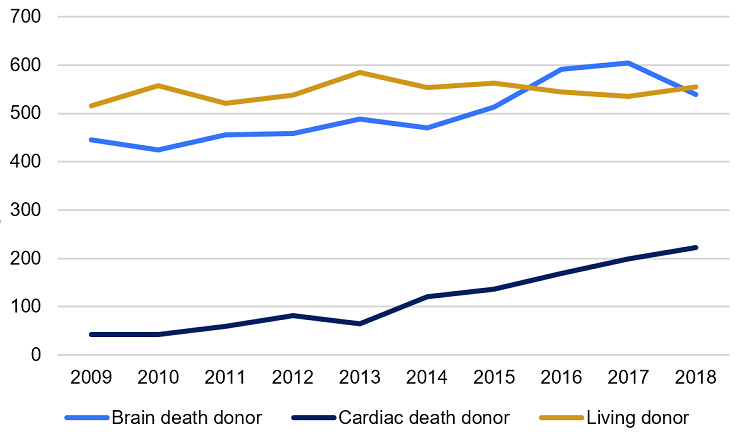
Within Canada, British Columbia, Ontario and Quebec have the highest deceased organ donor rates, while Manitoba has the highest living donor rate. International comparisons reveal that Canada falls within the top 20 countries for both deceased and living donor rates, however Canada’s rates are significantly below the rates of the top-performing countries, including those of the United States.
The pool of potential deceased organ donors is limited by several factors, including manner and location of death, age and the previous health status of potential donors. Efforts have been made in recent years to increase the pool of potential donors by including, for example, cardiac death patients in addition to brain death patients. As well, some individuals who choose to end life support efforts or choose medically assisted death may wish to become organ donors, and Canadian guidelines for these situations were released in 2019.
Despite an increase in the organ donor rate in Canada in recent years, there is still a long waiting list of Canadians in need of an organ transplant. This Background Paper provides an overview of organ donation across Canada; discusses organ donor rates in Canada and compares them with those of other countries; and summarizes organ transplant activity in Canada. Information about the regulation of organ donation in Canada and strategies used to increase organ donor rates in various jurisdictions are discussed in a companion Library of Parliament publication by the same author, entitled Strategies to Optimize Organ and Tissue Donation and Transplantation. 1
In 2001, the Government of Canada announced the creation of the Canadian Council for Donation and Transplantation (CCDT), an advisory body to the Conference of Deputy Ministers of Health, in support of efforts by the conference to coordinate federal, provincial and territorial activities relating to organ donation and transplantation. The CCDT established standards and clinical practice guidelines with respect to cardiac death, severe brain injury, immunological risk following transplant and medical management to optimize donor organ potential.
In 2008, the CCDT ’s functions were transferred to Canadian Blood Services (CBS), which assumed responsibility for Canada’s organ and tissue donation and transplantation system. 2 In Quebec, the organization mandated to coordinate organ donation is Transplant Québec. Its mission includes both optimizing the availability of organs and coordinating their procurement and allocation. 3
When considering trends and statistics in organ donation, as well as when making comparisons of these figures among jurisdictions, it is important to keep a number of variables in mind. A low donor rate, for example, may be more reflective of lower rates of injury and better health care interventions than it is of a lack of altruism or poor recruitment of donors. Similarly, an ever-growing waiting list for organ transplantation may indicate that patients are surviving longer while waiting than they once did, rather than a worsening supply of organs for transplant. The following is a discussion of Canada’s performance in organ donation and transplantation in recent years, and how that performance compares with that of other nations.
Before discussing donor rates, it is important to note that there are different types of donors. For the purposes of this document, the following definitions apply to donors:
According to the Canadian Institute for Health Information (CIHI), the deceased donor rate in Canada increased by 42% between 2009 and 2018, from 14.5 to 20.6 donors per million population (pmp), which translates to 487 deceased donors in 2009 and 762 deceased donors in 2018, 4 although 2018 saw a decrease in the number of deceased organ donors by 41 compared to 2017. Overall, the greatest increase in the number of deceased organ donors has been realized since 2013. 5 Each deceased donor can provide up to eight organs, although the average number of organs used for transplantation in Canada is lower. 6
In large part, donations from deceased donors follow brain death, the traditional criterion used to determine the death of an individual. Brain death is referred to by CIHI as “neurological determination of death,” or NDD. 7 However, since 2006, donors have been recruited under certain circumstances after cardiac death. Organ donation following cardiac death is referred to by CIHI as “donation after cardiocirculatory death,” or DCD. 8 (Cardiac death is discussed further in section 3.3 of this paper, “Identifying the Donor Pool.”)
The number of deceased donors in this category has increased steadily since 2006, when there were only four DCD donors, all from Ontario. By 2010, all jurisdictions except Manitoba and Saskatchewan were considering DCD donors, and 45 DCD donors were procured that year. 9 Now, all provinces are equipped to recruit DCD donors, and the number of DCD donors has increased by 429% between 2009 and 2018. By 2018, this category accounted for close to 30% of all deceased donors and is largely responsible for the increased rate of deceased donors since 2008. 10
Some organs can be donated by living donors. Living donors can provide a single kidney, a partial liver (lobe), a single lung, a partial intestine (also called small bowel) or a pancreas (segment or islet cells). Living liver and kidney donations make up almost all living organ donations every year.
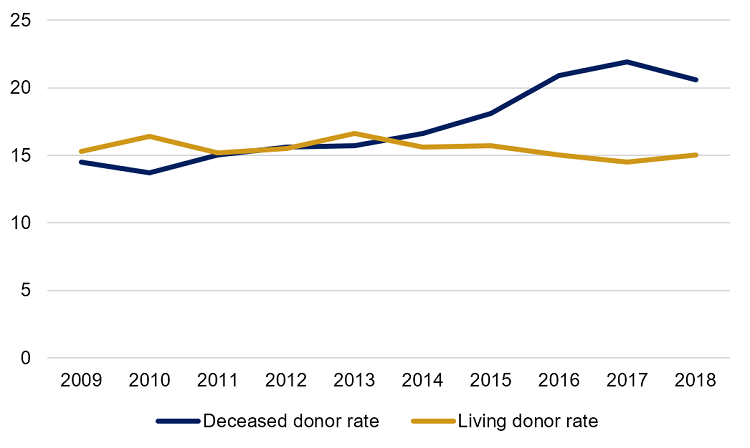
Between 2003 and 2012, the number of living donors in Canada grew from 435 to 539 and, until 2012, was greater each year than the number of deceased donors. 11 In 2012, the living and deceased donor rates were identical, at 15.5 pmp. Since 2014, the deceased donor rate has outpaced the living organ donor rate. Between 2009 and 2018, the living donor rate was at its lowest in 2017, at 14.6 pmp, 12 rising slightly in 2018 to 15.0 pmp, but with an overall decrease of 2% over those 10 years 13 (see Figure 1).
Figure 1 – Organ Donor Rates in Canada, 2009–2018 (per million population)
Source: Figure prepared by the author using data obtained from Canadian Institute for Health Information, “Figure 31: Donor rate per million population, by donor source, Canada, 2009 to 2018,” Treatment of End-Stage Organ Failure in Canada, Canadian Organ Replacement Register, 2009 to 2018: Donors – Data tables, 2019.
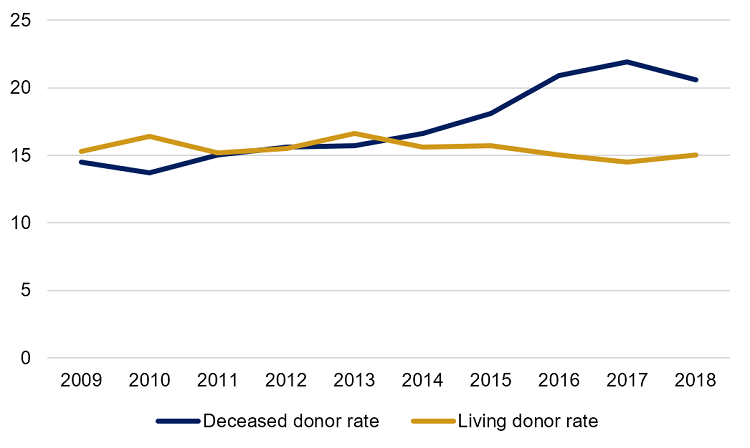
Figure 2 illustrates the trends in the number of deceased donors following brain death and cardiac death and the number of living donors, in Canada, from 2009 to 2018. The total number of deceased donors has increased over this time frame for both brain death donors and cardiac donors, while the total number of living donors has risen only slightly.
Figure 2 – Total Number of Organ Donors in Canada, by Type, 2009–2018
Source: Figure prepared by the author using data obtained from Canadian Institute for Health Information [CIHI], “Annual Statistics on Organ Replacement in Canada: Dialysis, Transplantation and Donation, 2009-2018 (738 KB, 9 pages),” CIHI Snapshot, December 2019, p. 5.
Figure 3 shows the living and deceased organ donor rates across Canada in 2018.
Figure 3 – Organ Donor Rates Across Canada by Region, 2018 (per million population)
Source: Figure prepared by the author using data obtained from Canadian Blood Services, Organ and Tissue Donation and Transplantation: System Progress Report 2018 (2.79 MB, 28 pages), 2019, pp. 12 and 14.
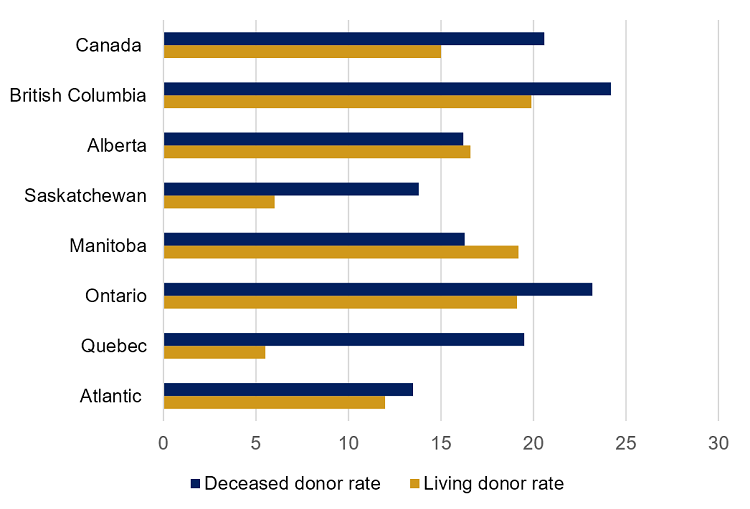
International comparisons of deceased organ donor rates reveal that Canada is not among the highest performers worldwide. In 2017, according to the International Registry in Organ Donation and Transplantation (IRODaT), Canada ranked 14 th among 70 countries for actual deceased organ donor rate, with a rate of 21.9 pmp. 14 However, Canada’s ranking among other countries fell in 2018 to 20 th , when the deceased donor rate was 20.6 pmp. 15 The top five countries in 2019 as listed by IRODaT are Spain (48.9 pmp), the United States (U.S.) (36.9 pmp), Croatia (34.6 pmp), Portugal (33.6 pmp) and France (33.3 pmp). 16 Canada’s 2019 deceased organ donor rate is not yet available.
Canada ranks better among other countries for recruiting living donors than it does for recruiting deceased donors. IRODaT ’s comparison of 2019 living donor rates put Canada in 14 th place for that year, at 15.0 pmp. In comparison, Turkey ranked first, at 53.0 pmp. The U.S. had a higher live donor rate than Canada, at 23.0 pmp, while Spain performed poorly compared to its actual deceased donor rate, at 7.2 pmp. 17
The disparity among donor rates can be ascribed to several factors. In addition to the specific organ donation and transplantation practices of each country, social, demographic and mortality characteristics can affect the pool of potential organ donors. As well, the calculation of the donor rate can change, depending on which definition of “donor” is used. The World Health Organization provides definitions for “actual donor,” “deceased donor,” “living donor” and “donor.” 18 Canada uses “actual donor” numbers, which include only donors from whom organs have been retrieved and successfully transplanted into recipients, to calculate its donor rate. Some countries may calculate donor rates using the definitions for “deceased donor” and “living donor,” which include those instances where a donor is identified and organs are retrieved, but ultimately no organ is transplanted into a recipient. This method inflates donor rates relative to Canada and other countries that use actual donor numbers.
Figure 4 provides comparative data of living and deceased organ donor rates in selected countries for 2018.
Figure 4 – Organ Donor Rates, Selected Countries, 2018 (per million population)
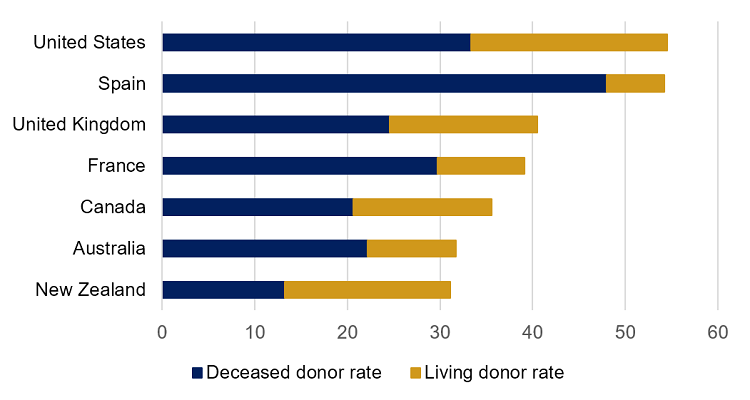
Sources: Figure prepared by the author using data obtained from International Registry in Organ Donation and Transplantation (IRODaT), “Worldwide Actual Deceased Organ Donors 2018 (pmp),” and “Worldwide Living Organ Donors 2018 (pmp),” International Registry in Organ Donation and Transplantation: Preliminary Numbers 2018 (375 KB, 14 pages), June 2019; and IRODaT , “Worldwide Actual Deceased Organ Donors Rate 2019 (pmp),” and “Worldwide Living Organ Donors Rate 2019 (pmp),” International Registry in Organ Donation and Transplantation: Preliminary Numbers 2019 (448 KB, 16 pages), March 2020.
Data from the Global Observatory on Donation and Transplantation for 2017 included, for the first time, a gender breakdown of donor rates for several countries, although Canada was not included. Globally, in 2017, deceased donors were 60% male and living donors were 52.5% female. In the U.S., deceased donors were 60% male and living donors were over 60% female, based on 2017 data. 19 CIHI reported that, in 2018, 60% of deceased donors were male and 63% of living donors were female, similar to the U.S. ratios. 20
There is a tendency to assume that all members of the general population are potential donors. However, the reality is such that few individuals will ever be in the situation of being considered for organ donation upon their death. Proponents of donor registries (databases containing the names of individuals who wish to donate their organs after death) suggest that such databases better reflect the donor pool. As with the general population, this is not strictly true, because the number of individuals who ultimately become available as potential donors is a small fraction of those who may be interested in becoming donors (intended donors).
Potential deceased organ donors are in fact identified from within the very limited pool of individuals whose death fulfills specific medical criteria. As mentioned in section 3.2.1 of this paper, this has traditionally meant that the individual would have succumbed to brain death, or NDD . Brain deaths are often the result of such incidents as trauma from a motor vehicle accident, a gunshot wound or a cerebrovascular accident, such as a stroke. The pool of potential donors has expanded slowly in recent years to include donation after cardiac death, or DCD . However, the cardiac death must occur in a hospital that is equipped to follow the candidate as a potential organ donor. Finally, within this limited pool, the number of candidates may further be reduced because of age. While there is no specific donor age cut-off in Canada, over the years, there has been a tendency to limit eligibility to individuals under a given age. However, the number of older organ donors has increased recently, as candidates are assessed on a case-by-case basis. 21
Information from CIHI indicates that in 2006, Ontario and Quebec were the first provinces to consider individuals who succumbed to cardiac death as organ donor candidates. Now, all jurisdictions in Canada consider organ donation following cardiac death. According to a 2017 study, the acceptance of organs following cardiac death in Ontario has expanded the donor pool and increased overall transplant activity. 22
Circumstances that could result in DCD include cardiac arrest in someone already brain-dead, unsuccessful resuscitation of a person in cardiac arrest, and cardiac arrest following withdrawal of treatment of an unconscious or incompetent patient whose death is anticipated. The last situation is referred to as “controlled DCD ” because preparations for organ removal and preservation can be initiated before the donor’s death, thereby controlling the timing of the withdrawal of treatment. 23
Developments in recent years have resulted in two new circumstances involving conscious and competent persons that may expand the pool of potential controlled DCD donors. First is the situation in which a person affected by an advanced neurodegenerative disease who is receiving life-sustaining measures chooses to have those measures stopped and to donate their organs. Second is the circumstance of a person who chooses medical assistance in dying (MAiD) and to donate their organs. These situations were not contemplated when the DCD guidelines were published in 2006. 24
In response to the need for additional guidance when considering recruitment of organ donors from these new categories, CBS , in collaboration with the Canadian Critical Care Society, the Canadian Society of Transplantation and the Canadian Association of Critical Care Nurses, published a guidance policy document in 2019 following consultation with medical, legal and ethics experts. The publication, entitled Deceased organ and tissue donation after medical assistance in dying and other conscious and competent donors: guidance for policy, makes several recommendations and provides the clinical pathway to follow for both circumstances. 25 Briefly, the key recommendations address the following issues:
According to CBS , 1,317 individuals, living and deceased, donated organs in Canada in 2018, and 2,829 transplant procedures were performed. While there was a 23% increase in annual transplants performed in 2018 compared with 2009, the rate fell by 6% between 2017 and 2018 as a result of a similar drop in deceased donors. 27 Of the 1,709 kidney transplants performed in 2018, 486 were from living donors and 1,223 were from deceased donors. Kidney transplants have always made up the largest proportion of organ transplants. Other organ transplants performed in 2018 included liver (535 transplants, including 69 from living donors), lung (361 transplants), heart (193 transplants) pancreas (11 transplants) and combination kidney-pancreas (48 transplants). 28 While there were no intestinal transplants reported in 2018, CIHI reports that there have been 55 intestinal transplants (excluding Quebec) performed between 1999 and 2018. 29 The average number of organs used for transplantation from deceased donors, where multiple organs are available for transplant, fluctuated between 3.4 and 3.7 per donor from 1999 to 2008. 30 The average number of organs transplanted per deceased donor has continued to fall. In 2018 only 3.0 organs per deceased donor, on average, were transplanted. 31 CIHI notes in its annual statistics for 2018 that fewer transplant procedures were performed in 2018 than in 2017 (2,782, or 148 fewer than the previous year), 32 which is consistent with the lower deceased organ donor rate for 2018 (20.6 donors pmp versus 21.9 pmp in 2017). 33
Despite Canada having a considerably lower organ donor rate than Spain’s, in 2017, the transplant rates for deceased donor lung and pancreas and living donor kidney and liver transplantation were higher than in Spain, while the rates for heart transplants in the two countries were similar. 34 Data from the Global Observatory on Donation and Transplantation reveal a gender disparity in transplant recipients. Although Canada has not provided a gender breakdown of transplant recipients, the global data for 2017 suggest that there are nearly two male transplant recipients for every female (63.2% versus 36.7%, respectively). 35
Five-year survival rates in Canada following organ transplantation are generally high and have improved modestly since 2009, mostly in terms of kidney and liver transplants. Survival rates following kidney transplant are higher for living donor kidneys than for kidneys from deceased donors. As of 2018, 88.0% of adult patients who received a living donor kidney were still alive five years after the transplant, while 81.3% of adult recipients of kidneys from deceased donors were still alive. 36 Five-year survival rates among pediatric patients is higher, at 94% and 89%, respectively. 37 Five-year survival rates for lung transplants is the lowest at 66.6%, while over 80% of heart, liver and pancreas transplant recipients survive at least five years. 38
As discussed in section 3.2.3 of this Background Paper, Canada does not include in its donor rate calculations potential donors whose organs were not used (either because the organs were not recovered, were not viable or were not transplanted). There are numerous reasons why organs are not used, only some of which can be controlled and possibly targeted as areas through which organ donor rates could be improved. For example, while non-use because of organ damage or other anatomical damage or poor organ function are reasons that cannot be overcome, logistical problems experienced by the donation and transplant teams and failure to search for or locate potential recipients are circumstances that could be addressed.
The logistical issues and identification of compatible recipients could be improved with an information management system like the real-time national waiting list operated by the private, not-for-profit United Network for Organ Sharing (UNOS) in the U.S. 39 through the Organ Procurement and Transplantation Network (OPTN). Created under the National Organ Transplant Act of 1984, the OPTN links all professionals involved in the donation and transplant system by maintaining the national waiting list and allocating donated organs based on “equity in access to transplants.” 40 All U.S. transplant centres and organ procurement organizations are members of the OPTN .
In 2018, 223 Canadians died waiting for an organ, and at the end of the year, 4,351 people were awaiting an organ transplant. 41 In 2017, 242 people died, and 4,333 people were awaiting transplants at the end of the year. 42
As long as there is a gap between the number of organs available for transplantation and the number of organs needed, it will be necessary to explore options for increasing both the deceased and living donor rates. Potential strategies to increase the number of organs available for transplant are discussed in a companion Library of Parliament publication by the same author, entitled Strategies to Optimize Organ and Tissue Donation and Transplantation. 43
Canada’s deceased organ donor rate has increased by 42% from 2009 to 2018, while the rate of live organ donors has declined slightly in the same period (by about 2%). Canada does not rank within the top-performing countries of those surveyed by the International Registry in Organ Donation and Transplantation with respect to organ donor rate. Despite the increase in the number of organs available for transplant in Canada in recent years and the resultant increase in the number of transplants performed annually, there are still thousands of Canadians on the waiting list for an organ transplant, and hundreds die every year while waiting for an organ to become available.
† Library of Parliament Background Papers provide in-depth studies of policy issues. They feature historical background, current information and references, and many anticipate the emergence of the issues they examine. They are prepared by the Parliamentary Information and Research Service, which carries out research for and provides information and analysis to parliamentarians and Senate and House of Commons committees and parliamentary associations in an objective, impartial manner. [ Return to text ]
* This Background Paper is based on an earlier publication by the same author: Sonya Norris, Organ Donation and Transplantation in Canada, Publication no. 2018-13-E, Parliamentary Information and Research Service, Library of Parliament, Ottawa, 14 February 2018.
© Library of Parliament